At HealthIMPACT Forum NYC, Dr. Rasu Shrestha of Advocate Health shared how the nation’s largest hospital-at-home program is rewriting the future of healthcare — moving care beyond hospital walls into homes and communities. From pandemic-born innovation to a person-centered, digitally connected care model, this borderless approach is delivering better outcomes at lower costs while reimagining what modern healthcare can be.
Dr. Sejal Hathi, Director of the Oregon Health Authority, shares her journey from battling chronic illness to shaping groundbreaking healthcare policies. From revolutionizing Medicaid to integrating social determinants like housing and nutrition, Oregon’s approach is setting the bar for health equity. Dr. Hathi’s insights on the intersection of technology and healthcare delivery highlight how the state is making healthcare more accessible, affordable, and effective for all.
In this article, we explore how generative AI is unlocking solutions for rare diseases. By accelerating drug discovery and enabling personalized treatment, AI is transforming healthcare for underserved patient populations. Advanced data analytics play a crucial role in addressing the complexities of diagnosing and treating rare conditions, providing new pathways for effective solutions and improving patient outcomes.
In this enlightening discussion, we explore the transformative concept of aging in place through a holistic healthcare lens. The conversation delves into the benefits of allowing seniors to live independently in their homes while receiving comprehensive support tailored to their unique needs. We uncover the vital role of technology, community engagement, and interdisciplinary care teams in creating an empowering environment for older adults. This dialogue highlights innovative strategies that promote emotional well-being, enhance quality of life, and ensure that aging in place is a realistic and fulfilling option for everyone.
Discover how telemedicine revolutionizes addiction treatment with patient-centered design. Learn about improved accessibility, continuity of care, and patient empowerment in this innovative approach to overcoming substance use disorders. Explore the future of digital health solutions in addiction care.
In an interview at HealthImpact Live, Janae Sharp and Dr. Chris Gibbons discussed the evolving digital health industry, the dangers of bias and blind faith in generative AI tools, and the steps needed to rebuild patients' trust in digital health systems. Dr. Gibbons emphasized the importance of data transparency and the need to address bias in AI training models. He also highlighted the need for doctors to assist in the design of AI algorithms directly. Dr. Gibbons expressed optimism about the future of digital health and emphasized the need for collaboration to improve patient experiences and outcomes.
As we head to HIMSS this week, we are reflecting on the highlights from the ViVE conference. The HealthIMPACT team was able to attend the ViVE conference in Los Angeles. We were looking for the good news in healthcare, and we were not disappointed. Here are five of our highlights.
Discover the benefits of multi-cloud adoption in healthcare and the importance of disaster recovery solutions. Learn more at HealthIMPACT Live.
Dr. Jitendra Barmecha, CIO of SBH, discussed the challenges of being a CIO in the healthcare industry in a recent interview with Janae Sharp. Dr. Barmecha addressed the issues of interoperability and staffing, emphasizing the need for cross-training, resilience, and business continuity planning during the COVID-19 pandemic. He also highlighted the impact of the pandemic on the industry, which accelerated the digital capabilities of healthcare organizations. Despite the constantly evolving landscape, Barmecha believes that healthcare CIOs can drive positive change and improve outcomes for patients and communities by focusing on digital capabilities and meaningful information at the point of care.
The Trusted Exchange Framework and Common Agreement (TEFCA) is a nationwide network that enables authorized parties to exchange medical records. In a recent interview, Dr. Micky Tripathi, Director of the Office of the National Coordinator for Health Information Technology (ONC) at the US Department of Health and Human Services, discussed the potential impact of TEFCA on healthcare in the US, highlighting the need for a common set of terms and conditions and the importance of digital workflows in healthcare transactions. The interview covers the timeframe for organizations to apply for the exchange framework and the scope of information that will be exchanged, including the US Core Data for Interoperability (USCDI), which includes basic medical record information supported by all electronic health record vendors and providers in the country. TEFCA aims to streamline health information exchange, enable secure and efficient data exchange, and help break down data silos. However, some health system leaders have expressed concerns about the potential costs and technical challenges of implementing TEFCA, as well as the potential impact on patient privacy and data security. While TEFCA is a significant step towards achieving interoperability, a comprehensive approach involving technology, policies, and incentives is needed.
The 10th Annual HealthIMPACT Forum was held in New York on January 25th. The keynote speaker, Gail Zahtz, shared her personal story of surviving late-stage cancer and how it led her to become the CEO of WiseCare Heal. Her talk emphasized the need for healthcare leaders to make decisions that serve patients, providers, and the business of healthcare.
Gail called for a shift in the culture of healthcare organizations from selling a "service of sickness" to sharing responsibility for the health of entire populations. She stressed that to succeed in the shift from fee-for-service to value-based care, a change in culture is needed and healthcare organizations should partner with companies who sell and service solutions for providers.
Gail's story and call to action highlight the importance of making healthcare more patient-centered and the need for ongoing reform in the industry.
Workplace safety in healthcare settings, particularly in light of the COVID-19 pandemic and now, involves careful coordination. Todd Larson, an expert in workplace and public safety at HonorHealth, highlights the need for a culture of safety, effective training, and the use of technology to improve communication and prevent workplace violence. Using a digital command center to monitor safety performance in real-time and predict potential hazards is critical for success and increases safety. Creating a safer work environment and preventing incidents of violence against healthcare workers starts with culture.
An unprecedented number of innovative technologies were deployed in response to the sudden need and rapid expansion of virtual health during the pandemic. Two years in and we have a strained healthcare system and a tired workforce. The need for ingenuity and effective change remains. Explore with us the cultural, practical, and paradigm shifts necessary to ensuring your organization not only recovers but thrives in this era of medical management modernization as we all emerge anew.
The shift to virtual care during the pandemic has necessitated unprecedented approaches to patient experience and engagement challenges. Managing the health of vulnerable patients with chronic illnesses like diabetes virtually is of particular concern. Emily Dumas, Manager of Care Transitions at the University of Alabama Birmingham Medical Center, discusses the need for engaging accessible tools, and what works and what doesn't work when it comes to supporting, engaging, activating, coaching, and ultimately partnering with patients.
Global Healthcare Leader Yan Chow, MBA, and Tyler Stowell, Senior Director of Healthcare Revenue Cycle Management, both of Automation Anywhere, discuss the formidable challenges and potential automation solutions to comply with the No Surprises Act.
With the initiation of the No Surprises Act, the burden shifts to the payer and providers to negotiate payments before the patient is sent a bill. With staffing shortages, this can be a huge challenge for back offices. Dr. Chow and Tyler illustrate how leading health systems are using RPA and intelligent automation to address these new regulatory challenges and realize dramatic benefits, including administrative efficiencies, greater workload capacity, error reduction, and significant cost savings.
Data is generated at every point in the patient’s healthcare journey. How this data is protected, shared, governed, and used is paramount both to patient and business outcomes.
No matter how robust your organization's security stack is, vulnerabilities to intrusions still exist. Unmanaged cyberthreats can compromise your organization’s ability to perform its mission by putting critical assets, data, and services at risk. As more and more organizations move toward the cloud, keeping track of where sensitive data resides becomes increasingly difficult putting increasing pressure on data security teams. Melissa Lawlor, Director of Security GRC, of Hackensack Meridian Health, Dr. Mauricio Angee, Chief Security Officer, of the University of Miami, and Michael Ebert, Partner at Guidehouse Cyber Security Leader, discuss how healthcare organizations can competently manage critical privacy and security issues.
There’s no question that we’re facing a paradigm shift in healthcare, only where changes will stick and how we will shape the future of healthcare. How patients, providers, and healthcare leaders approach healthcare as a whole has changed. Our expectations of what we want and expect from contact with the health system, what a “safe” distance, procedure, or interaction looks like, and how satisfied each participant is with an increasingly digital experience of healthcare are wildly different than they were a year ago. True transformation is always a result not just of the availability of new technologies, but also of the willingness of patients, providers, and health systems to adopt it, and insurers to pay for it. This sea change of expectations has the potential to be the most transformative aspect of our new world.
The digital divide continues to result in inequitable healthcare and healthcare access — particularly for people with disabilities. Historically, people with disabilities have not been part of the conversation, let alone, involved in the development of healthcare technologies “from the ground up.” According to Dr. Brook Ellison, PhD, of Stony Brook University, it is estimated that 1 in 4 people either have short-term or long-term disabilities. People with disabilities often have complex medical and healthcare access needs that are not addressed.
Dr. Ellison, Valerie Mondelli of RevSpring, Kimberly Noel, MD MPH of 23andMe, and Jan Smith Reed of T-Base Communications, discuss how providing differently-enabled patients with bad technology effectively disables them, and how adaptive technologies can make a vast difference in access and quality of care.
Organizations must combat inequity by better meeting patients where they are. As healthcare leaders, we are only just beginning to understand the importance of inclusivity when conducting a structural assessment of your institution’s readiness for doctors and patients with disabilities. As organizations struggle to support clinicians’ mental health and address burnout post-pandemic, it is important to explore ways to make the profession accessible to physicians with disabilities. Dr. Poullos, founder and Co-Chair of the Stanford Medicine Abilities Coalition (SMAC), a group composed of people with disabilities and their allies at Stanford Medicine, shares his vision for a digitally-enabled inclusive healthcare system and how organizations can combat inequity by better meeting patients where they are.
This discussion focuses on building an effective digital care strategy to meet the new challenges in a pandemic world. We cover viewpoints on the changing business model, what to expect with the shift to virtual care, and impacts on organizational strategy. Plus, we discuss the proactive measures you can take to thrive in the post-COVID business environment. How are technology budgets allocated, and is the way things have always been the way they should be going forward?
Will Patterson, CEO of CareRev, and Mark Smith, VP of Workforce Strategy & Analytics from Providence Health, discuss strategies to improve the work environment and give healthcare professionals the work-life balance they are seeking. By shifting the healthcare labor paradigm with efficient on-demand models, health systems meet staffing challenges by tapping into overlooked & underutilized talent pools. Harness and extend the potential and power of your existing workforce, minimizing the challenges of onerous onboarding, credentialing, and training processes to speed up access to work.
Exhausted and overwhelmed, clinicians are reaching a breaking point as the COVID-19 pandemic enters yet another phase. Physicians have less autonomy, while suffering in unsupported environments. Technology developed to improve treatments, remote communication, and clinical data collection have become additional burdens to bear. Dr. Vivian Pender, President of the APA, Dr. Jon Ripp, Chief Wellness Officer at the Icahn School of Medicine at Mount Sinai, and Anthony Giordano VP at Sermo sat down to discuss how clinicians in an ever-changing workforce can adapt technology to encourage peer to peer connection, reduce burnout, and how building a refreshed healthcare system starts with leadership and listening.
Burnout among clinicians is skyrocketing, driven by increasing documentation and technology inefficiencies. Sandra Powell-Elliot of Hackensack-Meridian Health notes it is not only a matter of quality of life but impacts the way human resources are pulled from patient care. So what challenges prevent innovation at the hospital level? Vishnu Saxena, Digital General Manager Healthcare Northern America of Dedalus, joins the conversation to discuss the way AI can help optimize time, improve patient care, and prevent burnout.
AI-powered digital front-door technology helps patients determine what their medical needs are, where to find the care they need, and subsequently aids with scheduling. This technology creates a better patience experience and frees up valuable provider resources. Our panelists Stefan Behrans, Co-Founder and CEO of GYANT, and David Fletcher, AVP of Telehealth Geisinger, discuss the challenges of this new technology as well as the opportunities.
Phreesia's Director of Clinical Content Dr. Alicia Cowley and Senior Product Manager Rachel Goldman provide an overview of Phreesia's end-to-end COVID-19 Vaccine Management Solution. Effectively manage outreach, intake, reminder & recall tools to increase vaccine uptake and address COVID vaccine hesitancy.
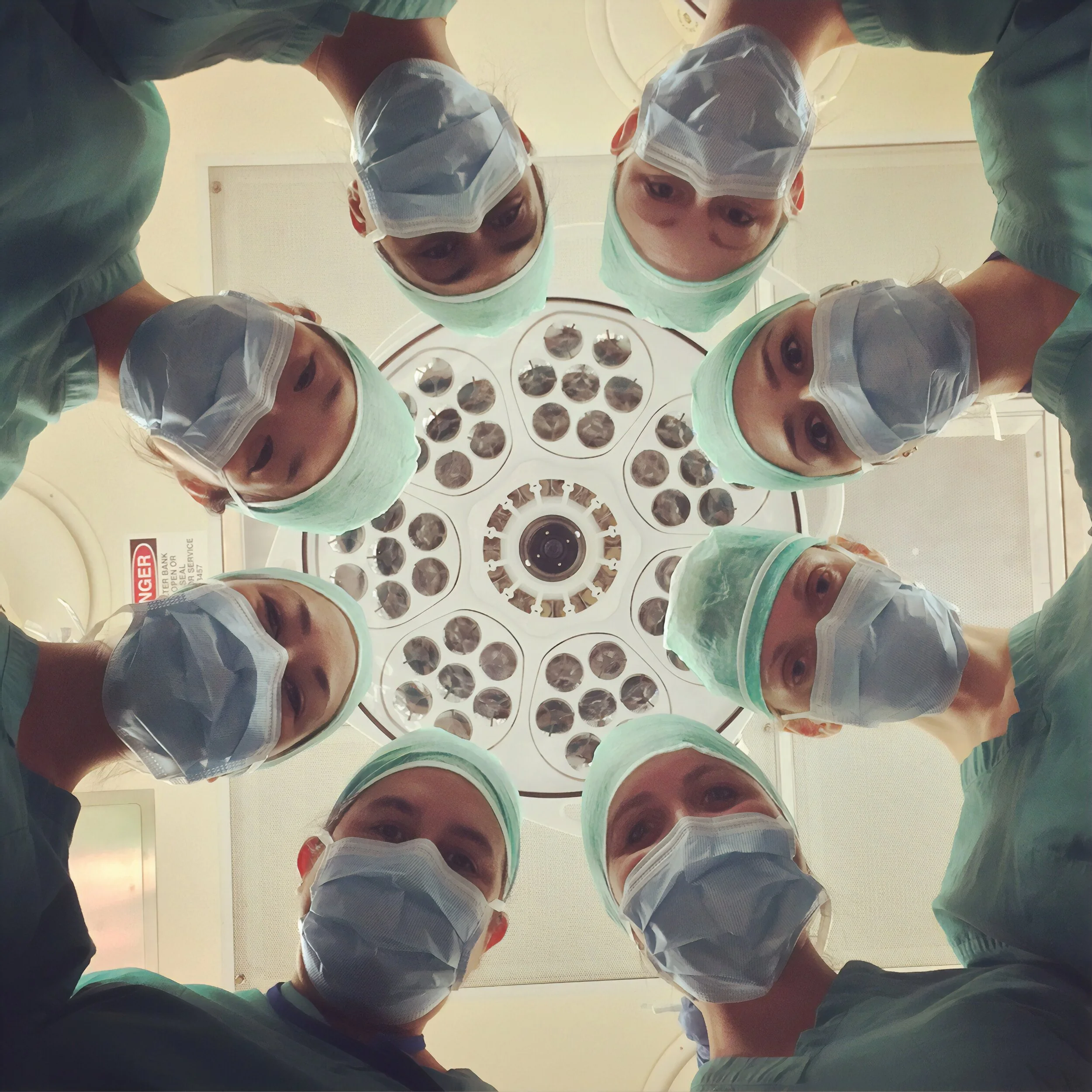
Telemedicine enables industry and outside clinical experts to participate live in the operating room without having to physically be there.
Daniel Hawkins, CEO, of Avail MedSystems, demonstrates how leveraging technology improves the efficiency inside of med tech as well as inside of hospitals, while driving down medical & operational costs.
COVID-19 has illuminated in stark relief how vast disparities in social determinants affect health care access and outcomes. Care and coverage (or lack thereof) can upset not just individual lives, but communities and economies as well. The pandemic is highlighting the need for a comprehensive public health approach that requires leadership, evidence, clear communication, and community cooperation. Momentum is building to rethink healthcare through the lens of what it means for our society at large. “We know there are huge health disparities,” states Leana Wen, MD, MSc, and Public Health Professor at George Washington University. In her discussion, she speaks about the opportunity to make lasting change.
During the COVID pandemic, an unprecedented number of innovative technologies were deployed, at scale - within weeks, challenging long-held biases regarding remote technologies.
Join us on the frontier of patient access and adoption as we explore in this panel discussion the top lessons learned from CXO’s, from: rapid testing, changes to EHR’s, re-configuring wards, retraining staff, requisitioning new materials, and more…




























In the generative AI era, a new Harris Poll survey reveals that two-thirds of U.S. hospitals entrust CIOs to acquiring data analytics platforms. This highlights a significant shift in strategic leadership roles within healthcare organizations. However, the survey also underscores the challenges and opportunities of this transition.